Hi, I am S.Sai Srija , 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
A 60 year old woman ,farmer by occupation R/O Suryapet came to the OPD on 11th September with the chief complaints of
Fever since 1 month
Headache since 1 year
Cough since 10 days
Cold since 15 days
Back pain since 1 year
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 1 year back then he developed headache and back pain since 1 month ,fever since 1 month and cough since 10 days.
Headache : It is in parietal region,continuous and relieved on medication.It was associated with nausea and giddiness on walking.
It is radiating to neck and spine
Fever :It is of high grade, continuous,not progressive,with no diurnal variations and is associated with chills and rigor.
Cold : It is intermittent,aggrevated during cold climate and relieved on medication
Cough : It is intermittent and is associated with sputum which is thick and white in colour,with no postural variations and is associated with wheezing.
PAST HISTORY:
Not a known case of HTN/DM/Asthma.
No H/O blood transfusion and no drug allergies.
No C/O loose stools,nausea, vomiting
No C/O chest pain,orthopnea
No C/O burning micturition.
No C/O increased or decreased urinary output
FAMILY HISTORY:
Not significant
PERSONAL HISTORY:
Diet-Mixed
Loss of appetite since 1 month
Sleep - Adequate
Bowel,Bladder movements-regular
PHYSICAL EXAMINATION:
GENERAL EXAMINATION:
The patient is conscious,coherent,
Cooperative.
Well oriented to time,place and person.
Pallor -No
Icterus-No
Clubbing - No
Cyanosis - No
Lymphadenopathy-No
Pedal odema- No
BP :130/70mmHg
PR :88bpm
RR : 20cpm
SYSTEMIC EXAMINATION:
CVS:
S1,S2 heard
No murmers
Respiratory system:
Wheeze is present
Central position of trachea
Normal vesicular breath sounds
Abdomen:
Shape of abdomen-Obese
No organomegaly
No palpable masses
No scars
CNS :
No focal neurological deficits
INVESTIGATIONS:
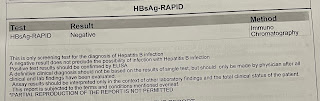
CBP: