Hi, I am S.Sai Srija , 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
A 40 year old male patient, farmer by occupation R/O Lingotam came to the OPD with the chief complaints of
Pain in abdomen since 3 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 days ago after which she developed pain in abdomen, squeezing type,insidious in onset and gradually progressive.
H/O of alcohol binge 3 days back,then he had 5 -6 episodes of loose stools and then pain in abdomen started.
No H/O vomitings
No H/O chest pain,Shortness of breath
PAST HISTORY:
N/K/C/O HTN/DM
H/O similar complaints 2 months back
FAMILY HISTORY:
Not significant
PERSONAL HISTORY:
Diet- Mixed
Appetite-Normal
Sleep -Adequate
Bowel and bladder movements-regular
PHYSICAL EXAMINATION:
GENERAL EXAMINATION:
The patient is conscious,coherent,
Cooperative.
Well oriented to time,place and person.
Pallor -No
Icterus-No
Clubbing - No
Cyanosis - No
Lymphadenopathy-No
Pedal odema- No
Vitals :
BP :150/90
PR :606pm
RR :14cpm
SpO2:99%
SYSTEMIC EXAMINATION :
CVS:
S1,S2 heard
No murmurs
Respiratory system:
No wheeze
Central position if trachea
Normal vesicular breath sounds
Abdomen:
Tenderness- epigastrium and umbilical region
No palpable mass
No scars
No organomegaly
Central Nervous System:
No neurological deficits
INVESTIGATIONS:
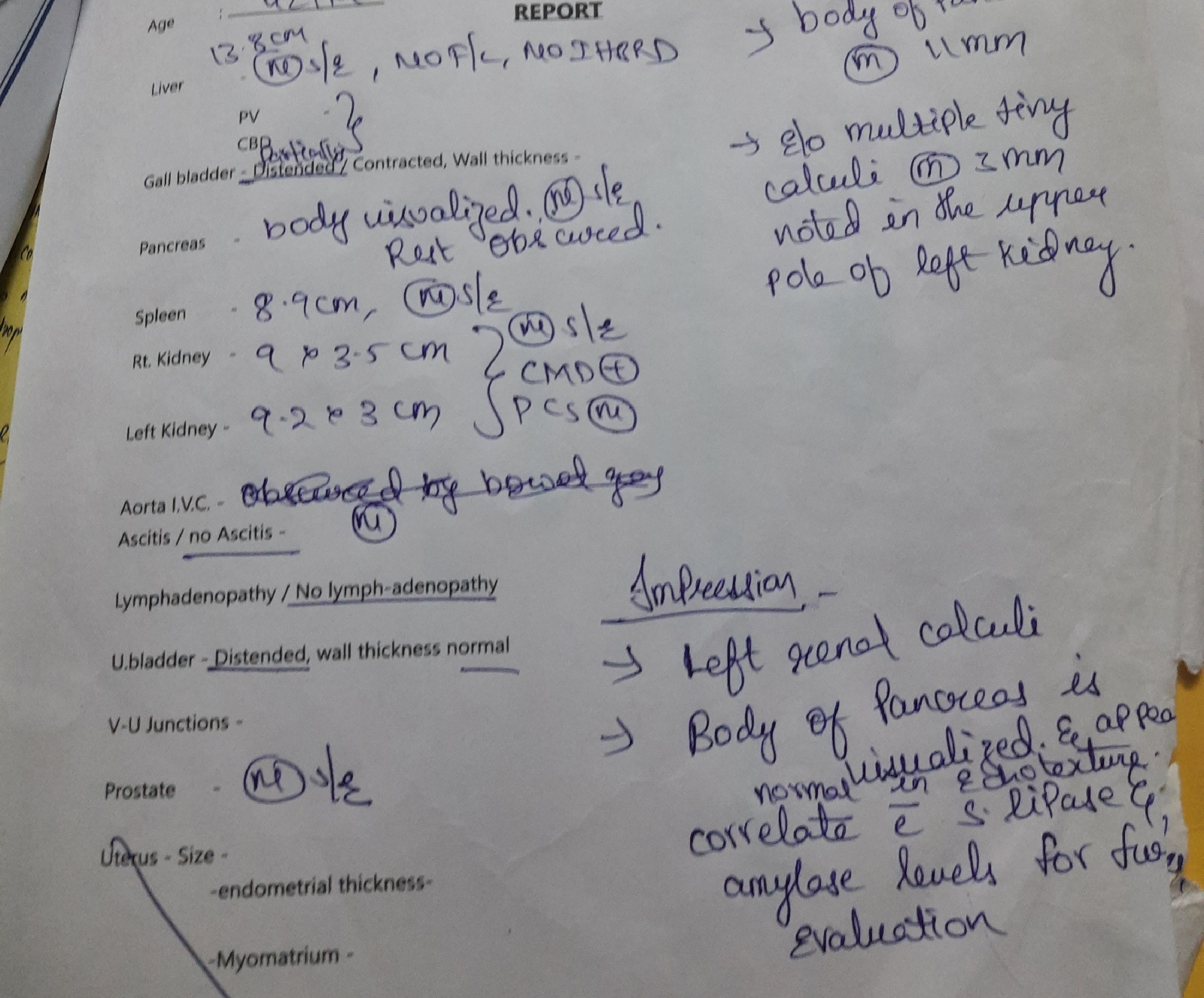
Ultrasound: